Battle Of Nerves
Severe lumbar spinal stenosis is no walk in the park
The beauty of walking is that an exercise so simple could have so many benefits—improved circulation, better bone and muscle mass, and balance. But it’s not so simple for people with lumbar spinal stenosis. For them, walking hurts.
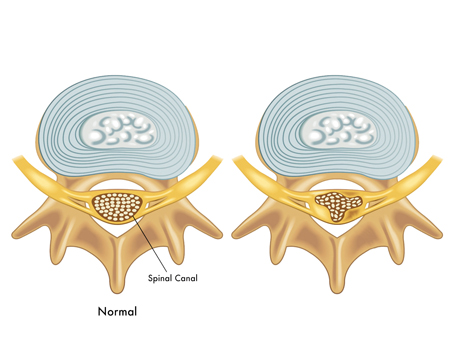
The pain of lumbar spinal stenosis actually comes from the nerves in the spinal canal, or other passages in the spine, being compressed or constricted. This is because the spinal canal has narrowed through degeneration, often due to normal aging, or from osteoarthritis, which involves the breakdown of cartilage in the joints and can cause the development of bone spurs. The narrowing of the canal is called stenosis.

The Lumbar Spine
“The low back, or lumbar area, is made up of five individual bones located below the rib attachment of the thoracic spine, but above the sacrum and pelvic bone,” explains Davis Reames, MD, a neurosurgeon at Neurological & Spine Institute. “In contrast to the relatively rigid thoracic spine bound anteriorly by the rib cage, it allows for substantial spinal motion. Unfortunately it is also the most common source of spinal pain.”
Along with the leg pain caused when walking, patients with lumbar spinal stenosis may feel pain or numbness in their lower back or buttocks. The pain can often be relieved by sitting down or resting, but who wants to be bound to a chair by their nerves?
“Leg pain can be severely disabling and often can stop us completely in our tracks, affecting our jobs, our family, and negatively impacting our quality of life,” Reames says. “Fortunately, there are effective treatment options.”
Diagnosis And Early Treatments
Providing a detailed history and undergoing a thorough exam will help your physician determine if your leg pain is caused by lumbar spinal stenosis or a different condition. Patients will also need to receive an MRI or CT scan.
“It is important to see a specialist who can best uncover the severity of the nerve damage, complete a careful review of the images with respect to your specific complaints, and finally maintain a wide variety of techniques with which to consider, in order to choose the least invasive treatment to best provide you with relief,” Reames says.
Conservative treatments for lumbar spinal stenosis include medications for inflammation and nerve pain, including cortisone injections in the lumbar spine. Physical therapy and lifestyle modification can also help in some cases.
When Surgery Is Needed
“If the pain is severe or refractory to conservative methods, or if other signs such as weakness are present, surgery may become indicated,” Reames says.
Lumbar decompression surgery is done to remove the sources of compression on the nerves. Traditionally, this surgery involved a large incision to access the spine and surrounding tissue. But for certain candidates, Dr. Reames prefers to perform a minimally-invasive decompression.
“In this procedure, a small tube is carefully placed under sequential dilation which, instead of a large incision that requires more soft tissue and muscle injury, only temporarily splits the longitudinal muscle fibers rather than disconnecting them from their attachment at the bone,” Reames explains. “This is done through a small 18-millimeter incision under the guidance of imaging. This allows a microscope to assist in carefully removing bone spurs, disc herniations, cysts, or other nerve impingement. As in standard open surgery, the nerves are clearly visualized at the conclusion of the operation. Dermabond glue is then placed on the skin and patients are sent home the same day.”
For patients whose quality of life has become so hampered by this condition that a procedure is needed, this minimally-invasive technique helps keep spinal surgery from being a last resort.
“The patient benefits from a decreased rate of infection, less blood loss, and a quicker recovery,” Reames says. “In fact, for appropriate surgical candidates, some degree of immediate improvement in leg pain is expected in the recovery room.”